Congenital diaphragmatic hernia (CDH) is a life-threatening birth defect. It is an abnormal opening in the diaphragm, resulting in the baby’s organs rising from the belly into the chest. This negatively affects lung growth and how the lungs work after birth. As a result, 30% of all babies born with this defect who do not have other abnormalities, die because of limited lung function. Especially in severe forms of CDH, the survival rate is currently still very low. Today’s standard of care is planned delivery followed by intensive neonatal care. Once the baby is medically stable, the defect in the diaphragm is closed surgically.
Over the past decades, a team of researchers at the University Hospitals Leuven developed fetal surgery (surgery before birth) to increase the survival rate of babies affected by CDH.
Survival rate more than doubled in severe cases
The research team has now completed a large randomized clinical trial. This type of research is recognised as the gold standard to provide the best evidence for a new form of treatment. The trial included 289 pregnant women who were carrying a baby affected by a moderate or severe form of congenital diaphragmatic hernia. The pregnant women were randomly allocated into two groups. Babies in the first group received surgery before birth, the second group received no surgery before birth. After birth, all babies received standard intensive care, including repair of the defect.
Prof. Dr. Jan Deprest, gynaecologist at the University Hospitals Leuven and principal investigator of the consortium: “The survival rate of babies with a severe diaphragmatic hernia has more than doubled by the surgery before birth: it was 40% in the group that received fetal surgery, compared to a 15% survival rate in the group without surgery before birth. Therefore, we will now offer fetal surgery as a standard treatment option in the University Hospitals Leuven for babies who have a severe form of the birth defect. Of course, the choice of treatment remains with the parents.”
The survival rate of babies with a severe diaphragmatic hernia has more than doubled by the surgery before birth: from 15% to 40%.Prof. Dr. Jan Deprest, gynaecologist
In moderate cases of CDH, in which babies have a 50% chance to survive, there was a trend for improved survival (+13%), but the gain was much smaller.
The researchers further confirmed that this type of fetal surgery is safe for the mother. Earlier research had already shown that the operation before birth does not cause reproductive or gynaecological problems later on.
Premature birth
A disadvantage of fetal surgery is the need for a small incision in the womb. That incision may cause rupture of the membranes and amniotic fluid to leak out. This may, in turn, trigger premature delivery and can counteract the effect of fetal surgery. Researchers now aim to improve the procedure to further reduce the risks. In the more moderate presentation of the disease, the team aims to further determine the subgroup of babies for which fetal surgery is most beneficial. To additionally improve the survival rates for CDH, the Leuven team is also investigating drugs that can be taken by the pregnant woman to further improve lung growth in the fetus.
About the procedure
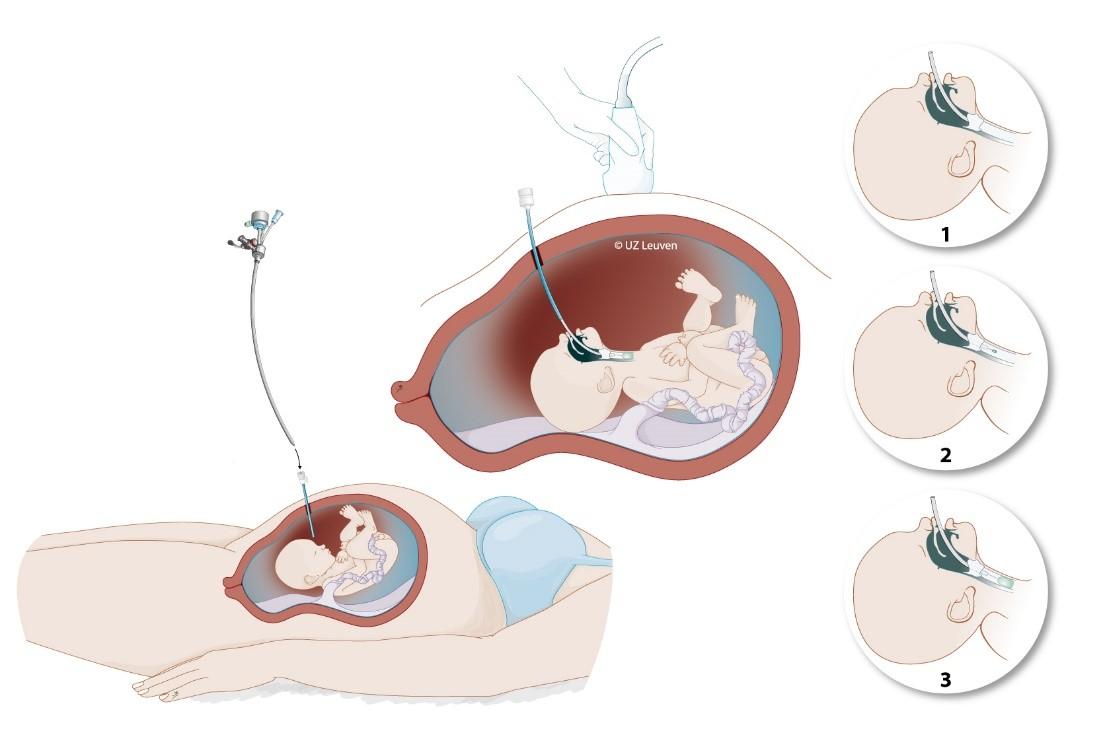
The surgery is called FETO or Fetal Endoscopic Tracheal Occlusion. It requires a 3-mm cut under local anaesthesia in the belly of the pregnant mother, after which a very small camera is inserted into the womb and then into the baby’s windpipe (trachea). The baby receives an injection for pain relief. Next, a small balloon is inserted and inflated to block the windpipe, to stimulate the baby’s lungs to grow. During pregnancy, the baby’s lungs do not contain air but produce most of the fluid in the womb. Temporarily blocking the windpipe leads to a build-up of the fluid in the lungs, which stimulates their growth. A few weeks later in pregnancy, the balloon is removed to allow the lungs to mature and to unblock the windpipe.
In addition to existing procedures for spina bifida and for placental division in the case of identical twins, this study now provides evidence that fetal surgery also improves the outcome for babies with congenital diaphragmatic hernia. The University Hospitals Leuven performs more than 140 fetal surgeries per year, the majority of which on patients from abroad. Fetal surgeries are carried out and followed up by a multidisciplinary collaboration between the departments of fetal medicine, neonatology, paediatrics, surgery, anesthesiology and the center of human genetics.
The team acknowledges the patient organisations CDH UK (United Kingdom) and PlatformCHD (The Netherlands & Flanders) for their help in the successful completion of this trial and informing perspective parents.

