Life-saving procedure
Pulmonal endarterectomy, or PEA for short, is a complex but life-saving procedure for cardiac patients with chronic thromboembolic pulmonal hyertension (CTEPH).
CTEPH results from pulmonary emboli (blood clots in the bloodstream to the lungs) that are not broken down by the body but scarred. The scarred tissue starts to completely or partially clog the pulmonary vessels, forcing the heart to pump much harder to send blood through the blood vessels of the lungs. As a result, blood pressure in the lungs gets abnormally high. If untreated, CTEPH will continue to get worse: if pressure in the pulmonary vessels continues to increase, it can lead to reduced heart pump function and eventually even to heart failure. A successful procedure lowers or normalises pressure in the lungs, which leads to improved fitness and a higher life expectancy of the patient.
Technical feat
During the six-hour procedure, the chest is opened via sternotomy, splitting the sternum in half lengthwise. Next, the heart-lung machine temporarily takes over the function of the heart and lungs. The pulmonary artery is surgically opened after which the inner wall, including the scarred blood clots, is carefully removed. To be able to do this, the patient is cooled down to 18° C with the help of the heart-lung machine. This allows not only the heart, but also the heart-lung machine itself, to be stopped for a while and the pulmonary arteries to be completely free of blood. Afterwards, the patient is rewarmed, the patient's heart starts beating again and the heart-lung machine is stopped.
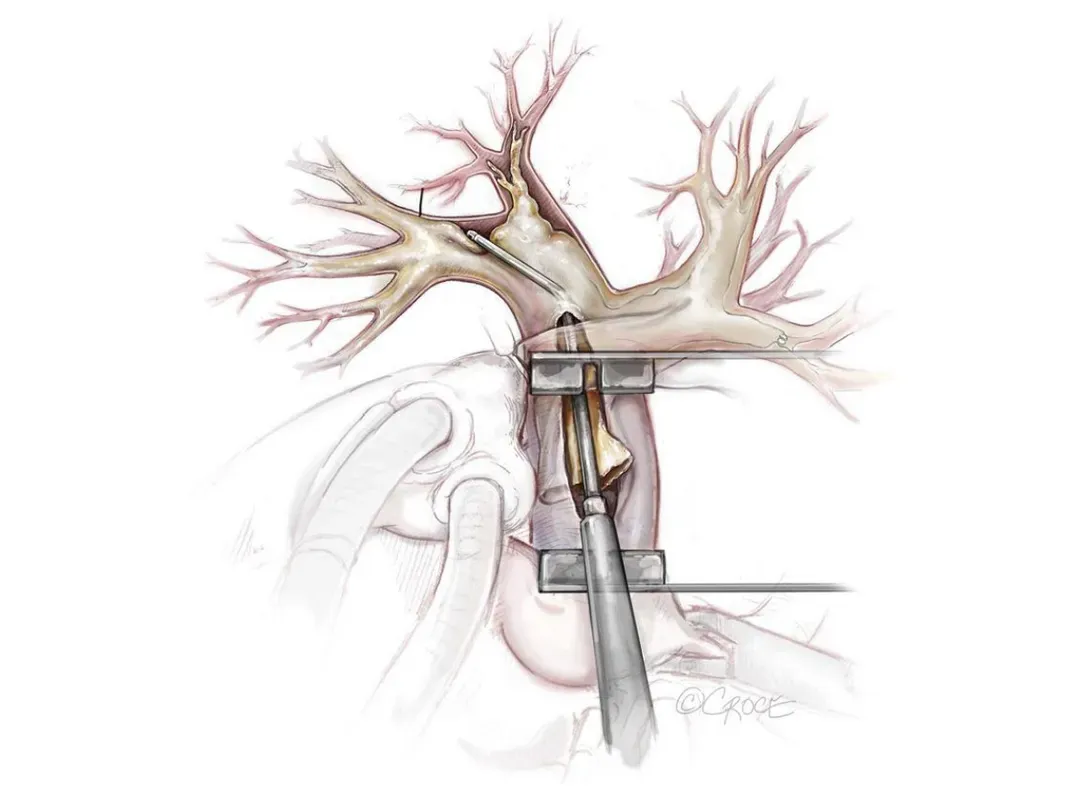
© Guth S, et al. Ann Cardiothorac Surg 2022:1 1:180-188.
Increasing number of procedures
On 14 June 2024 the surgical team performed its three hundredth PEA surgery at UZ Leuven since its inception in 1999. In those 25 years the annual number of PEA procedures has been increasing steadily: from nine in the first ten years to twelve in the following decade. The last five years there were some 17 procedures a year. 2023 was a record year with 25 procedures.
The programme was initially set up by prof. dr. Marion Delcroix and the first procedures were performed by prof. dr. Willem Daenen. In 2006, cardiac surgeon prof. dr. Bart took over the programme and since 2018, prof. dr. Tom Verbelen performed the last 110 procedures.
By talking to the referring doctors, I hope to increase knowledge and raise awareness about CTEPH and to increase the number of PEA procedures. Prof. dr. Tom Verbelen
Prof. dr. Tom Verbelen
Prof. dr. Tom Verbelen, cardiac surgeon and cardiac surgery deputy head of clinic: “Together with better centralisation of care, it remains UZ Leuven's ambition to achieve the target of 33 procedures per year in the future. According to current guidelines, an expertise centre needs to perform at least 50 PEA treatment a year and have a mortality rate of less than 5 percent. But recently we have determined a 'volume outcome' based on scientific literature. This showed that an expertise centre should at least perform 33 PEA treatment a year, rather than 50. By talking with referring doctors, I'm hoping to increase knowledge and raise awareness about CTEPH and to increase the number of PEA procedures. And even though we are currently still performing less than 33 procedures a year, I am proud that our mortality rate in planned procedures is lower than 4% putting us on a par with the largest centres worldwide.
Lung embolism
In pulmonary embolism, a blood vessel in the lungs becomes blocked by one or more blood clots. These can originate from the blood vessels in the limbs or the abdomen after a thrombosis and then be carried along with the blood flow that reaches the lungs via the heart. Usually a pulmonary embolism can be easily treated with anticoagulants, but one or more blood clots may also fail to dissolve properly. This, in turn, can lead to CTEPH.
Every year, 1 in 1,000 Belgians suffer a pulmonary embolism. Approximately 3 percent of the patients develops CTEPH. So every year, there are about 199 new patients with CTEPH in Belgium.
Prof. dr. Verbelen: “A pulmonal endarterectomy is one of the procedures I prefer to perform. On the one hand because of the surgical technical challenge and because of the of the often immediately noticeable result in the patient. On the other hand, because it is a nice example of a multidisciplinary care programme: pulmonologists, cardiologists, radiologists, interventional radiologists, cardiac surgeons, anaesthesiologists, intensivists but also nurses, perfusionists, nursing specialists and physiotherapists are all involved. I sincerely hope that the efforts from the team can result in a further increase in the number of procedures in the future.”
Centralising care
Centralising care mean concentrating medical care and treatments for certain conditions or patient groups in a specific location or at a specialised medical centre. The objective of centralisation is improving quality of care by pooling expertise and means in one location.
