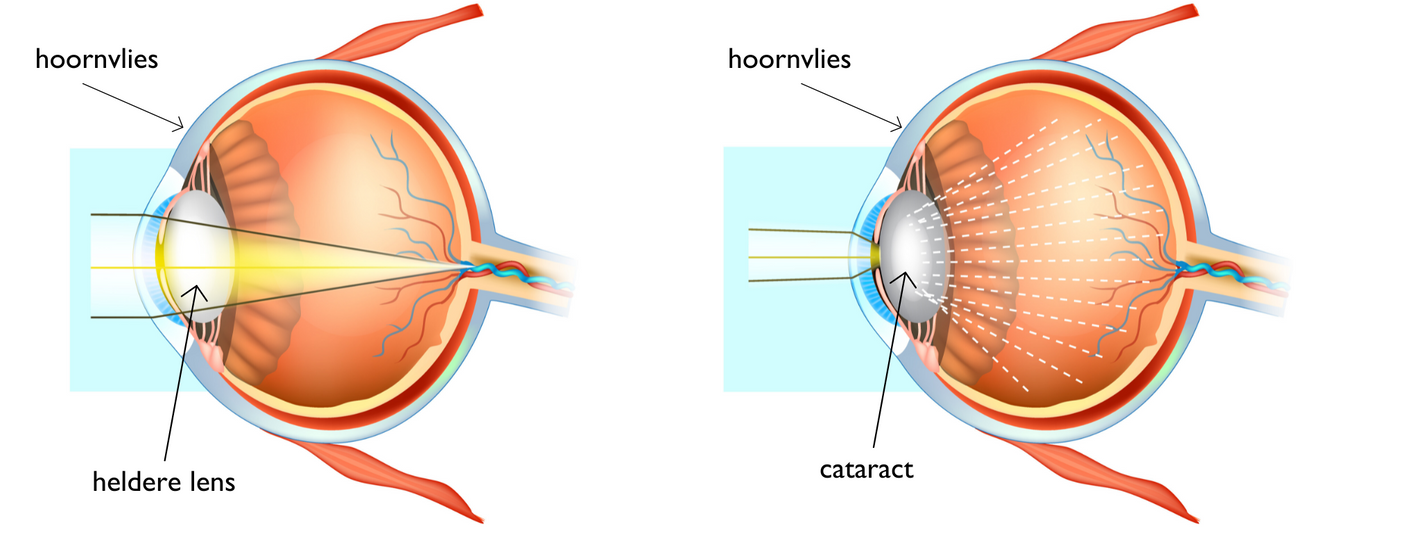
What is cataract?
Cataract, or clouding of the eye’s lens, reduces the clarity of the lens, leading to blurred vision.
Cataract is typically an age-related condition, but children can also develop it at a young age.
When the lens is clouded from birth, it is referred to as congenital cataract.
How common is it and what are the causes?
Children under one year of age
Cataract occurs in approximately 1 in 10,000 children under the age of one.
In very young children, identifying the cause can be challenging. To determine this, the ophthalmologist collaborates with paediatricians and the human genetics centre.
If cataract affects both eyes, the child may have had an infection during pregnancy (e.g. rubella) or may have an underlying genetic condition (trisomy 21) or a systemic disorder. Isolated cataract in both eyes can also be inherited from one generation to the next. With parental consent, a blood test is carried out to rule out certain causes.
If only one eye is affected by cataract, it is usually due to a developmental disorder affecting the eye’s blood supply and is rarely linked to heredity or a systemic condition.
Older children
A child may also develop cataract later in life, for instance, due to a blow to the eye (trauma) or after radiation therapy.
Treatment
Not all cases of lens clouding require immediate surgery. If an eye examination shows that the cataract is slowing down or preventing the child’s visual development, the ophthalmologist will decide whether surgery is necessary.
Procedure
The operation is performed under general anaesthesia. Therefore, it is essential for the child to fast before the procedure:
- Young children may have bottle feeding and/or breastfeeding up to 4 hours before surgery.
- Older children may have a light breakfast up to 6 hours before surgery.
During the procedure, the ophthalmologist makes tiny incisions in the cornea, only a few millimetres in size. Through these incisions, the cloudy lens is removed.
In young children, no artificial lens is implanted yet. The same applies if the eye is too small or has an abnormal structure. In such cases, the child will be left without a lens, a condition known as aphakia. In older children, an artificial lens is inserted during the operation.
All incisions are closed during surgery, either with self-dissolving stitches that disappear after six weeks or with sutures that need to be removed later.
Immediately after the procedure, the child receives an eye shield to protect the operated eye. This shield can be removed the day after the surgery.
(Read more under the images)
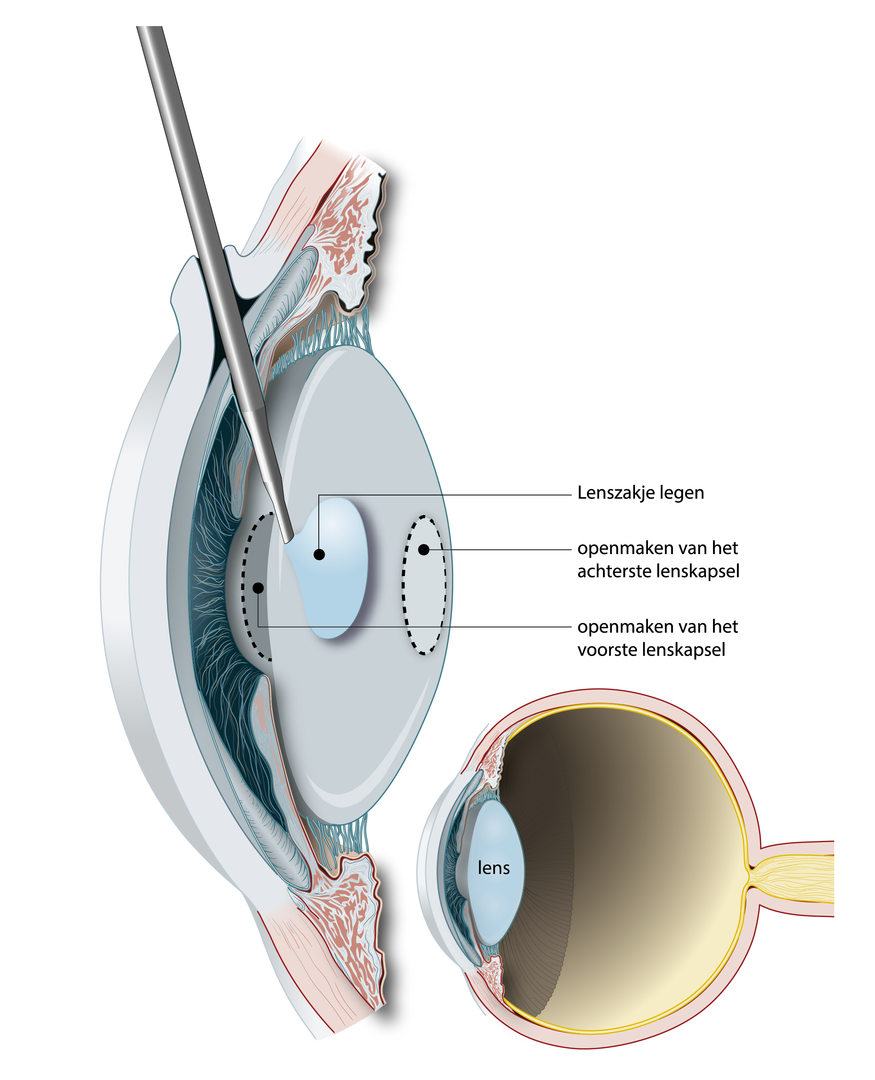
In young children, not only is the lens capsule emptied, but the posterior lens capsule is also opened.
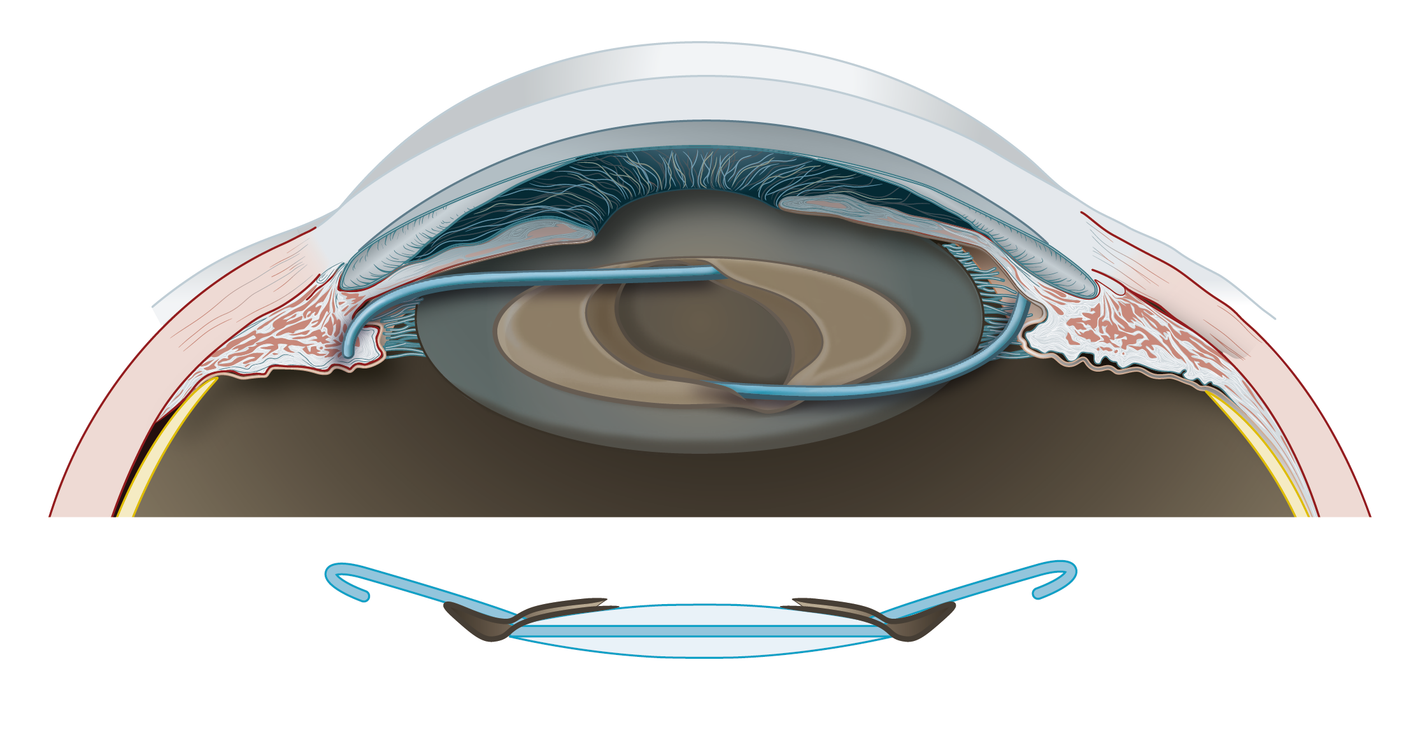
The lens implant is positioned with its arms in the sulcus (between the iris and the anterior lens capsule), while the optic part of the lens is placed behind the posterior capsule.
After the procedure
At home, the child must receive regular eye drops. This can be challenging, but the following method is the most effective:
- Lay the child flat on their back.
- Place a drop in the inner corner of the eye.
- The child will blink naturally, allowing the drops to spread into the eye.
The child must not rub their eye immediately after the drops have been administered.
For the first three months after the procedure, the child should not swim or play in a sandpit to prevent dirty water or sand from entering the operated eye.
Once the child has sufficiently recovered from the operation, they can return to nursery or school.
Final outcome
For children with cataract in both eyes, there is about a 50% chance of achieving 50% or better vision.
For children with cataract in one eye, vision in the treated eye may remain weaker than in the healthy eye, even after surgery and additional visual stimulation. There is about a 30% chance of achieving 50% or better vision. However, peripheral vision is usually much less affected.
Potential risks of the procedure
Short-term risks
The risk of infection after eye surgery is very low (less than 1 in 1,000). However, if an infection does occur, it can severely affect vision.
If the child experiences any of the following symptoms within four weeks of the procedure, contact the medical team immediately:
- Increased pain and/or redness of the eye
- Reduced drinking
- Vomiting
- Increasingly blurred vision
- Sudden loss of vision
- Clear fluid leaking from the eye
- Pupil that is not round
- Seeing black spots, black threads, and/or flashes of light
- Injury to the eye
Long-term risks
Secondary cataract
Babies and young children develop secondary cataract much more quickly than adults. This usually occurs between 4 and 12 months after the initial surgery. In young children, a second operation is then required, whereas in older children, a laser treatment may be sufficient.
Read more about secondary cataract.
Glaucoma (increased eye pressure)
Glaucoma is characterised by high intraocular pressure, which can damage the optic nerve and cause vision loss. Around 30% of children who undergo cataract surgery at a very young age develop glaucoma, often several years after the operation. If detected early, it can be treated with eye drops. In some cases, additional surgery is necessary.
Clear vision after surgery: glasses or contact lenses
Since the child’s natural lens has been removed, an artificial means of focusing is required, either through glasses, contact lenses, and/or an implanted lens.
The appropriate correction depends on whether an artificial lens was implanted during surgery.
If no artificial lens was implanted during surgery (aphakia)
The child will need glasses with thick, strong lenses to correct their vision. However, such glasses can be difficult for babies to wear due to their small nose and narrow head. An aphakic contact lens may be a suitable alternative.
If an artificial lens was implanted during surgery
The child will need glasses with a minor correction for clear vision. A multifocal or bifocal prescription is usually given from around 2.5 to 3 years of age.
Stimulating the weaker eye
After surgery, the child will usually need to wear an eye patch over one eye for a few hours a day. This helps to stimulate the weaker eye, often referred to as a "lazy eye." This post-operative treatment is crucial for proper visual development.

Contact lenses in children
Once the eye has healed after the procedure, a contact lens can be fitted.
A week after the operation, a follow-up appointment is scheduled, during which the specialist will teach the parents how to insert and remove the contact lens for their child. The younger the child, the easier this adaptation process tends to be.
Finding the right fit
The first year of wearing a contact lens can be intensive. Finding the right size may take some time: the lens should not move too much or fall out easily.
Regular check-ups are important to ensure a proper fit. The contact lens must be replaced every three months. During each check-up, the paediatrician will also assess the prescription. If a change is needed, it will be adjusted immediately.
It is best to insert the contact lens every morning and remove it in the evening, just like a standard contact lens. Once a baby becomes accustomed to this routine, it will also be easier at preschool age, when inserting and removing lenses becomes a daily habit, much like brushing teeth.
After removal, the contact lens must be cleaned and stored in contact lens solution.
Inserting the contact lens: how to do it?
Make sure you have good access to the child’s eyes while standing. Position them at a comfortable height, for example, on a changing mat placed on a table or dresser.
You will need both hands to handle the contact lens and the eyelids. That’s why we recommend doing this with someone else, especially during the first few days. The other person can hold the child’s head steady.
- Open the lens packaging.
- Wash your hands thoroughly with water and soap, then dry them completely with a clean, lint-free cloth.
- Hold the contact lens between your thumb and index finger of your dominant hand, close to the edge.
- Lightly fold the lens (like a taco), with the convex side facing upwards.
- Don’t worry: the lens will not tear easily.
- Use the middle finger of your free hand to hold the child’s upper eyelid up. Press the eyelid gently against the brow bone to prevent blinking.
- With your dominant hand holding the contact lens, slide the lens under the upper eyelid. Push the upper eyelid towards the eye using the index finger of your other hand and release your dominant hand.
- Now, with your dominant hand, let the lower eyelid glide over the lens.
Removing a contact lens: how to do it?
- Wash your hands thoroughly with water and soap, then dry them completely.
- Position your child in a way that is comfortable for you.
- Place the thumb of one hand on the upper eyelid and the thumb of the other hand on the lower eyelid.
- Gently press both thumbs down and slightly towards each other to lift the contact lens up and out of the eye.
Cleaning the contact lens: how to do it?
- Immediately after removal, place the lens with its convex side in the palm of your hand.
- Add a few drops of cleaning solution and gently rub the lens.
- Be careful not to touch the lens with your nails.
- After rubbing, rinse the lens with the same solution.
- Close the bottle of cleaning solution tightly after use.
- Fill the lens case with fresh contact lens solution every day.
- Only then place the cleaned lens in the case.
- Ensure that the lens is fully submerged in the contact lens solution.
Keep the lens case clean
A clean lens case is essential for the safe use of contact lenses.
Rinse the lens case daily with contact lens solution after inserting the lens. Then, wipe the case dry with a clean paper tissue and allow it to air dry.
The lens case should be replaced every three months.
Questions or complaints? Contact us
-
Schedule an appointment with your ophthalmologist if:
- The eye appears red or is painful
- The child is sensitive to light
- There is excessive tearing or discharge from the eye
The ophthalmologist will examine the eye for possible infections or loose stitches.
-
Before the procedure: tel 016 34 23 27 (questions about the procedure, appointment cancellation, late arrival, illness, or fever on the day of the procedure)
-
After the procedure (medical questions or concerns):
- during working hours: tel. 016 33 23 70 (ask to be connected to the day hospital surgery unit)
- after 18:00 or during the weekend: tel. 016 33 22 11 (ask to be connected to the on-call unit)

